Science can often be dry and cold, and many discoveries and inventions have come along only because of the human intervention factor. Childhood scoliosis braces have been around for ages and ages, however, some of the more advanced and more comfortable braces have come into fruition truly because of some sensitive individuals and their patients, one of which was the daughter of the inventor himself. Let’s take a look at the history of scoliosis bracing and we will clue you in on some surprising ways that more advanced and comfortable braces have been developed. There is nothing like actual personal experience even among the most experienced doctors and ortho specialists and we will soon see exactly what that means.

In fact, unfortunately even the most successful, devoted, and experienced medical professionals cannot beat actual experience with illness or other medical issues that have happened to themselves or close members of their family. For example, I know a devoted and beloved doctor who recently suffered from grave complications from a kidney transplant. These types of snags happen to only one in one hundred kidney transplant patients. This doctor who is thankfully improving has gained monumental knowledge in the field of kidney disease that he could have never learned in school.
Some of our heroes in the development of bracing for idiopathic scoliosis are Walter Blount, Bill Miller, John Hall Ralph Hooper, Jr. among other innovators in this field. This article will touch on the developers and the braces that they fabricated while trying to give the human side to bracing history. We also want to stress the importance of orthotists as opposed to doctors in the invention of the most effective scoliosis braces. Even if these professionals do not have an MD after their name, nevertheless they are the ones who actually have the right feeling and experience to make the correct brace for each person.
Dr. Walter Blout, Dr. Albert Schmidt & The Milwaukee Brace
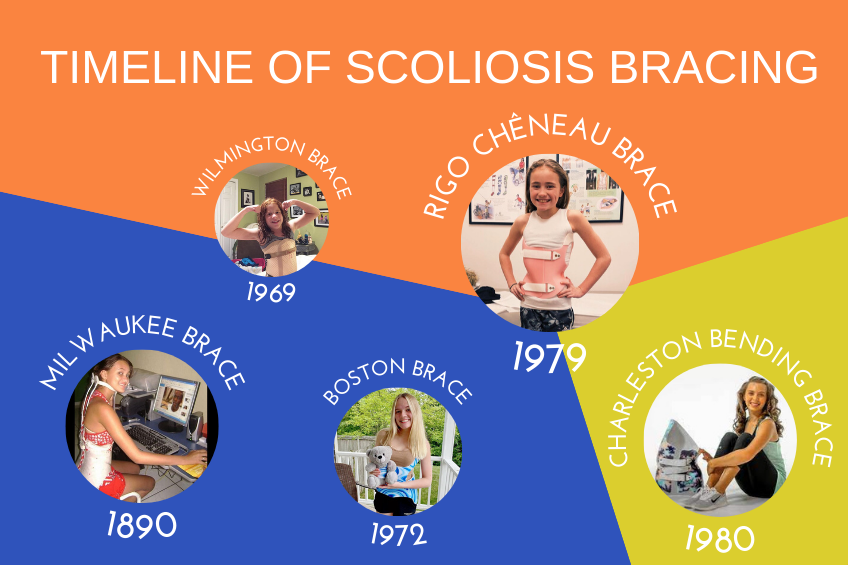
One of the first children’s scoliosis clinics in America to open was at Boston’s Children’s Hospital in 1890. The jacket/brace was made from plaster, rigid metal and included a neck ring. This was later called a version of the Milwaukee Brace. At that time in history, if someone wanted a non-surgical cure for adolescent idiopathic scoliosis this was the most common choice until the 1970’s. The child had to be fitted with a girdle, rigid metal rod and neck ring. This brace is still used today in certain instances for lumbar lordosis. It keeps the pelvis in a back tilting position using a pelvic corset made from leather. The rest of the brace is attached at an angle to a ring around the patient’s neck in which the throat mold is placed right under the chin and keeps the head in a certain position. It is quite a complicated appropriation.
G. Dean MacEwen & The Wilmington Brace
It wasn’t until 1969 that a better option was introduced. It’s so strange that nothing better was invented before 1969 to improve on the cumbersome Milwaukee Brace. Only because of a determined patient, a new brace called the Wilmington Brace was created. MacEwen was the chief of services at the Alfred I. Dupont Institute when he recommended the standard Milwaukee Brace in 1969 to a female patient. Low and behold, she refused this cumbersome contraception as well and only would agree to wear a brace that was undetectable even though, MacEwen tried offering her an alternative cast she was not buying.
At first, MacEwen thought that the girl’s request was quite unreasonable but with no alternative to save the child, he together with some other innovative colleagues created this removable brace. It fits like a jacket but has a front closure. It’s custom-made by using a plaster mold of the patient’s torso.
Bill Miller, John E. Hall and the Boston Brace
When a brave teenager who was a patient of John E. Hall and orthotist Bill Miller refused to wear a Milwaukee type brace; they were forced to design a less restrictive and more comfortable brace especially for this valiant teen. The Boston Brace is still used in a more modern model until today.

Bill Miller who was born in 1927 and died in 1992 founded Boston Brace in 1970. He was grabbed from his own successful orthotist business in Indiana to come to the Children’s Hospital in Boston where he created the Boston Brace. Bill jumped at the chance to develop new techniques in bracing because the Boston hospital was a branch of Harvard Medical School Teaching Hospital of which Hall was anxious to be a part of.
Dr. Hall and orthotist Bill Miller were the perfect combination to conceive the Boston Brace System for the purpose of treating scoliosis. The module that they designed was a thoracolumbar-pelvic innovation that came in different sizes and could be configured according to each person’s curvature and age. This idea might seem rudimentary today but, in those days, it was no less than revolutionary. The pressure areas would be specific to each person’s unique curvature.
Today there are a variety of Boston Braces that cater to each individual scoliosis sufferer.
The Boston Brace Original is still considered the main system for scoliosis with specific types custom-made for thoracic, lumbar or a combination of both problems. The standard brace comes with a back opening which gives optimal results consistently.
The Boston Brace Night Shift has gained popularity since it is worn exclusively while sleeping. This brace applies direct, oppositional forces to straighten the curves.
The Boston Brace Kyphosis Brace is used when there is an outward sway called, kyphosis when viewing the spine sideways or for lordosis which means an inward sway.
The Boston Brace RC is a custom-made asymmetrical brace with a front opening. It incorporates the style closely of the Rigo-Cheneau brace.
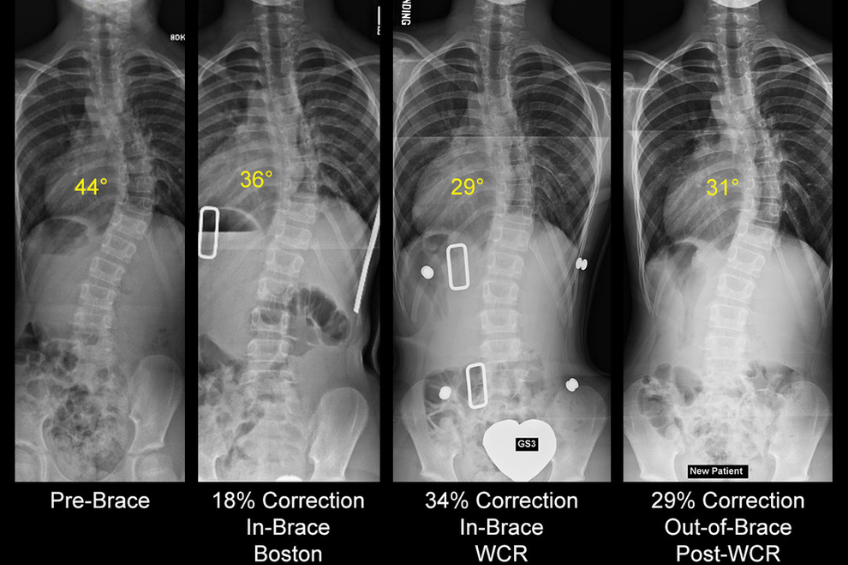
The Boston Brace 3D is the most up to date brace of all of Boston Orthotics bracing devices and ensures maximum curve correction. It is manufactured by utilizing a digital laser scanning system which measures the patient precisely. There are several other models used for other problems in babies or for people with low muscle tone which can be researched as well.
The Rigo-Chêneau Brace method is the gold standard throughout the world for the successful handling of idiopathic scoliosis thereby avoiding serious surgery.
C. Ralph Hooper, Jr. & The Charleston Bending Brace
Similarly, to Hall and Miller’s motivation for the invention of the Boston Brace, Ralph Hooper’s took a personal turn in l980 when his ten-year-old daughter, Jessica, was diagnosed with adolescent idiopathic scoliosis. Since her evaluation determined that she suffered from a right thoracic scoliosis she was not a candidate for the Boston Brace, and she would have to be fitted with the dreaded Milwaukee Brace. Jessica said something like, “No I will not wear that monstrosity on my neck.” Her father could not disagree since he had seen firsthand the damage that the Milwaukee Brace was having emotionally and socially to children suffering from scoliosis and having no alternative but that ring around the neck.
Jessica started out with a 30-degree thoracic curve, wore the new brace for two years with her curve reduced to a perfect zero. The Charleston Bending Brace can both conform to the child’s body and bend at the same time. Dr. Hooper admitted that the invention of this innovative brace was the highlight of his career. He made the Charleston Bending Brace especially for his daughter, Jessica and the results were amazing.
The way the Charleston Bending Brace works is that it is molded to fit the specific patient’s body while bending toward the curve while the patient is sleeping. That was the beginning of this innovation but with time patients were able to wear the brace for up to 23 hours a day.
Final Words
We have touched upon several bracing options for children suffering from scoliosis. There are other variations as well which should be presented as options to parents. What I have learned is that there is no such thing as the word no in inventing. So many revelations have been introduced by determined pioneers in all different fields. The common factor is a will to succeed. In the little bit of history, we introduced to you we showed you two ideas. Number one, “if there’s a will, there’s a way”. There is no better encouragement than a child who has a will of their own. It’s very hard to refuse a child when you know deep down in your heart that they are absolutely right. This was especially true in the case of Jessica, Ralph Hooper’s own daughter. How could he possibly refuse the one person he loves the most in the whole world?
The second idea is that it’s often the orthotist, not the doctor who is the expert on scoliosis bracing. Keep this in mind when researching the different options. A doctor can recommend the which brace and the orthotist will explain why that specific one.